Antimicrobial resistance (AMR) is one of the most pressing global health threats, and its implications are particularly critical in Southeast Asia. AMR occurs when bacteria, viruses, fungi, and parasites evolve to resist the drugs that once killed them or inhibited their growth, rendering standard treatments ineffective. This escalating crisis not only threatens individual health but also poses a severe challenge to healthcare systems worldwide, including in Southeast Asia.
What is AMR and Why Should You Care?
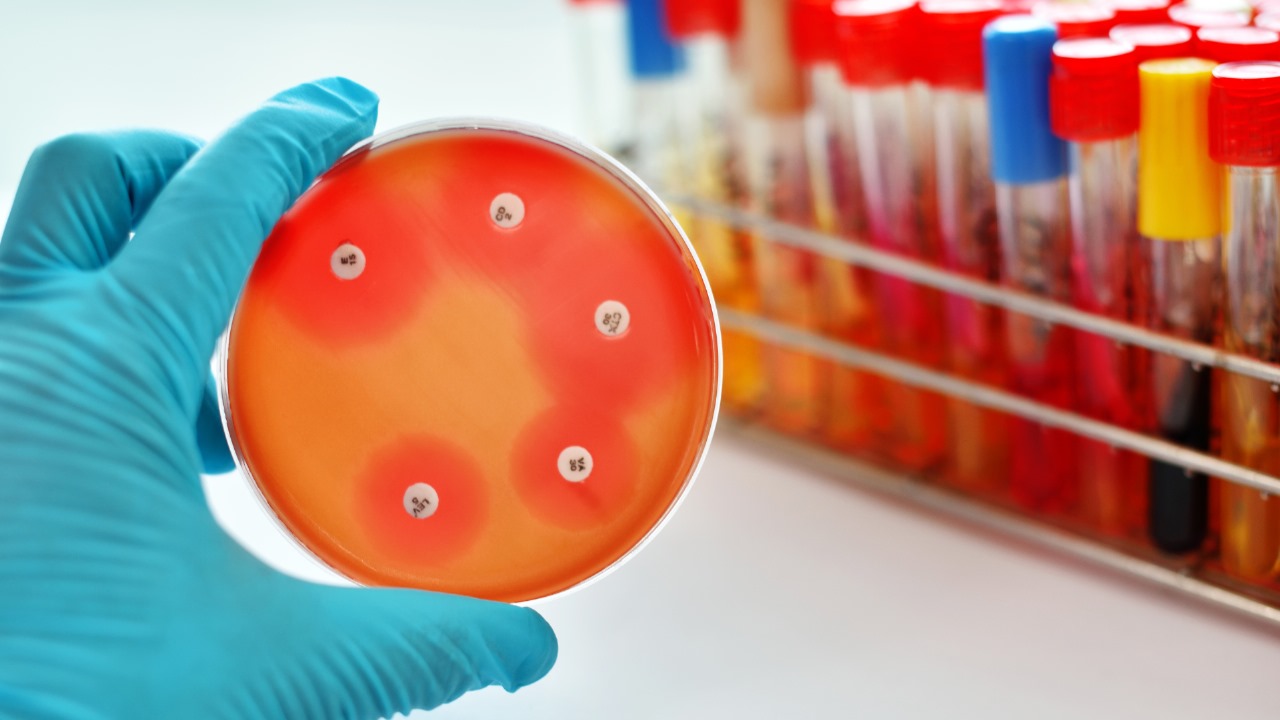
AMR refers to the ability of microbes (bacteria, fungi, viruses, and parasites) to resist the drugs that previously treated infections. For example, a patient with a bacterial infection that is resistant to antibiotics may face prolonged illness, a higher risk of severe complications, or even death.
In Southeast Asia, the situation is dire. The region has some of the highest rates of antibiotic misuse and overuse globally. This includes both the inappropriate use of antibiotics in human healthcare and their overuse in agriculture and animal husbandry. As a result, AMR is advancing rapidly, and its consequences are already being felt.
AMR and Its Impact on Healthcare in Southeast Asia
▪ Increased Mortality and Morbidity: With AMR, many infections that were once treatable with common antibiotics are becoming increasingly difficult to cure. Diseases like pneumonia, tuberculosis (TB), and urinary tract infections (UTIs) are becoming harder to treat, leading to higher mortality rates.
▪ Economic Burden: AMR strains healthcare systems, leading to longer hospital stays, more expensive treatments, and the need for more advanced (and often ineffective) interventions. This translates into higher healthcare costs, which can be a burden for
both individuals and governments.
▪ Threat to Medical Advancements: Many modern medical procedures, from cancer treatments to organ transplants, rely on effective antibiotics to prevent infections. The rise of AMR puts these procedures at risk, making previously routine treatments
more dangerous.
Why Is Southeast Asia So Vulnerable?
Southeast Asia faces a combination of factors that make it particularly vulnerable to the spread of AMR:
1. Overuse and Misuse of Antibiotics: Antibiotics are often available without a prescription, leading to over-the-counter misuse. Many people also take antibiotics for viral infections (e.g., colds or flu) where they are ineffective.
2. Self-medication: In some areas, people purchase antibiotics without proper medical advice, contributing to improper dosing and incomplete courses of treatment.
3. Agricultural Use: The overuse of antibiotics in farming (to promote growth in healthy animals) is contributing to resistant bacteria, which can then spread to humans through food or the environment.
4. Weak Infection Control: Inadequate hygiene, sanitation, and infection control practices in healthcare settings increase the risk of resistant infections spreading.
The Role of International Private Medical Insurance (IPMI) in Combating AMR
IPMI plans in Southeast Asia are critical in addressing the impact of AMR. By ensuring access to high-quality healthcare, these insurance policies can help mitigate the burden of resistant infections. However, they also have a role in promoting prevention:
1. Preventative Care: Many IPMI plans cover vaccinations, routine check-ups, and screenings that can help prevent the spread of infections, reducing the need for antibiotics.
2. Access to Expertise: With access to a global network of healthcare providers, IPMI plans allow patients to seek out specialists who can manage AMR infections more effectively.
3. Promoting Education and Awareness: Insurers can play a key role in educating their members about the risks of misuse and overuse of antibiotics. Many IPMI providers are already incorporating health awareness programs, aiming to reduce AMR risks.
4. Monitoring and Reporting: With IPMI, patients can receive guidance on the most effective treatments and benefit from the latest medical advancements that address resistant infections.
What Can Be Done to Tackle AMR?
Combating AMR requires collective action at the individual, community, national, and
global levels. Here’s what can be done:
▪ Awareness and Education: Increased public education on the dangers of AMR and the importance of proper antibiotic use is critical. This includes not self-medicating and completing prescribed courses of treatment.
▪ Strengthening Regulations: Governments need to enforce stricter regulations on the sale and distribution of antibiotics, ensuring that they are only available with a prescription.
▪ Improved Infection Control in Healthcare Settings: Hospitals and clinics must adopt stricter infection control protocols to prevent the spread of resistant infections.
▪ Promoting Alternatives: Research into alternative treatments, such as vaccines and new antibiotics, should be accelerated to stay ahead of resistant strains.
▪ Global Cooperation: AMR is a global issue. Countries must collaborate on research, share data, and strengthen international regulations to control the use of antimicrobial agents.
Why Act Now?
The window of opportunity to prevent AMR from becoming an even greater crisis is rapidly closing. The choices we make today will determine the health outcomes of tomorrow. By understanding the risks of AMR and taking decisive action, we can protect future generations from the consequences of ineffective medical treatments.
For individuals in Southeast Asia, it’s essential to not only protect your health with adequate International Private Medical Insurance but also to contribute to the global fight against AMR. Whether you’re in a large city or a rural area, every action counts. Now is the time to act before AMR makes common infections deadly again.